A CASE REVIEW OF A CALL AND WHAT WAS LEARNED
WRITTEN BY A FELLOW MEDIC
It was a typical hot summer night in Richmond when multiple calls were received about a shooting, seizure, or cardiac arrest, all clustered in the area of a local neighborhood. The exact location of the patient and the nature of the call was uncertain, but we had an address to start our search.
The police arrived first and confirmed this call did not include a victim of violence. The fire department arrived on the scene a few seconds after the police. Then we arrived on the scene to find a man lying in the mulch beside the sidewalk, police watching the scene, and fire department EMT’s examining the patient. The few bystanders who had called 911 said they didn’t know who the man was, but they witnessed him collapse while walking down the sidewalk. Additionally, the caller indicated the man was unknown to them. As a result they were unable to give any further information regarding his past medical history or the situation leading up to the call beyond what they witnessed including allergies, or medications. We had gotten the ambulance right against the curb. Fire reported that the patient was awake and probably drunk. They urged him to stand up, then supported him as his efforts were ineffectual, and placed him on the stretcher. My partner and I loaded the patient into the ambulance and told the fire department they were OK to go back in service.
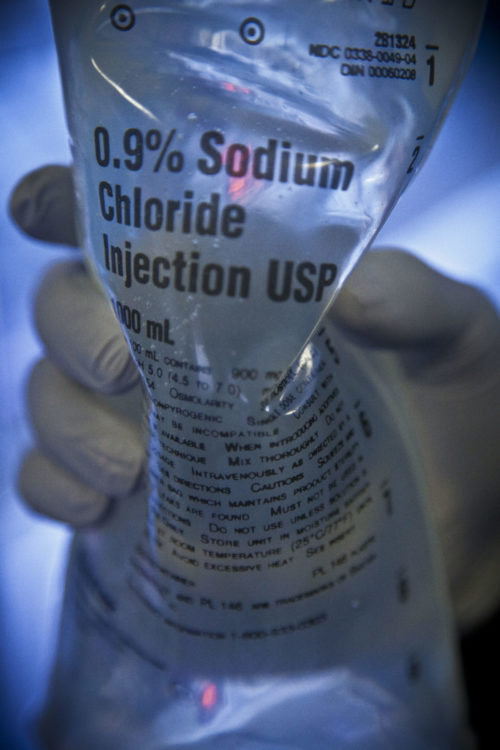
After loading him into the ambulance and attempting to engage with him, it was clear he had an Altered Mental Status (AMS) and was breathing quickly. His skin was dry and colored appropriately for his ethnicity. My partner immediately placed the blood pressure cuff and SpO2 sensor, and it started to register a heart rate. 180. Verifying this rate to the radial pulse, and inspected at the SpO2 waveform. The heart rate was correct, no doubt about it. My partner knew what to do next, and was already applying the cardiac monitor and 12 lead. Obtaining the IV start kit and placing an 18 gauge in his Left Antecubital fossa (LAC) while my partner finished the 12-lead. It was textbook supraventricular tachycardia (SVT), the patient responsive only to pain, not speaking directly to us. My partner obtained a blood sugar analysis, and the results were noted to be in the normal range. He then placed the combo pads on the patient, preparing for immediate synchronized cardioversion and then went outside to ask the fire crew to standby in case they were needed. We started a fluid bolus of normal saline, flowing wide open. I grabbed a drug kit and drew up Adenosine. My partner returned with two firefighters, and I explained the patient’s heart rate was high, and we would need to medicate the patient. With my partner positioned by the monitor and ready to engage the print button, I rapidly administered 6 mg of Adenosine and intently watched the monitor. The heart rate dipped down briefly to the 140s, P-waves visible, and then the heart rate returned to 180. There was no change to the patient’s heart rate, mental status, other vital signs. Then 12mg of Adenosine was prepared and administered with no positive effects noted.
At this point, I was at a crossroads. In retrospect, the patient’s vital signs, beyond the heart rate, respiratory rate, and mental condition, were acceptable. However, the altered mental state was looming large in my mind and the decision to cardiovert. After pre-treating with 5mg Versed IV push, the patient was syncronized cardioverted at 70 joules.
The patient’s arms flew up in the air. The patient spoke for the first time but then returned to an unresponsive state. The firefighters expressed surprise and questioned, “did he code?” No he did not code, what we did is called synchronized cardioverting. It was the same type of electrical treatment as defibrillation, but the initial shock was at a lower, much more specific setting. Turning my attention back to the patient, I saw that his heart rate was still high. I charged again and shocked again. We began to work through the “H’s and T’s,” and one of the firefighters asked if Narcan (Naloxone) would have any effect. I explained, Narcan would not treat the heart rate, and the patient’s breathing was fast, not slow. I charged to 100 joules and shocked again. The patient’s heart rate decreased to 148, and he began to respond to questions.
Next, I started a 150mg Amiodarone in 100ml D5W infusion over 10 minutes and told my partner to start heading towards the large academic level 1 trauma center for the City. I replaced the leaking bag of saline with a new one. The old bag, dumping its contents over the bench seat and the ePCR computer. Called in the patient report to the hospital so they could prepare for our arrival, stating the patient’s current condition and treatments performed. Further, explained the plan to cardiovert at 120, 150, and 200 joules, respectively, should the patient’s heart rate return to its previous levels. As if I had jinxed it, several minutes later the patient stopped responding to questions, and his heart rate returned to 180. At this point it was clear that the altered mental status was related to the heart rate. The patient was shocked at 120, 150, and 200 joules, stopping long enough between shocks only to confirm that the heart rate was still 180. Maxed out at 200 joules and then stopped. The Amiodarone infusion was nearing completion, and we were approaching the hospital. Called the hospital back and explained the heart rate had returned to 180, and that it was refractory to electrical therapy. In the hospital ambulance bays after transferring all my equipment to the stretcher, we began to move the patient inside.
While moving the patient inside it was noticed that the cardiac monitor was displaying a CPR feedback panel. Then, the truth was realized. There were no markers above the R waves on the EKG. The monitor was not synchronized. The patient had been defibrillated, not synchronized cardioverted, as intended. Felt weak and shaky of what could have happened, but by the grace of God did not. We continued to move the patient into the “critical” section of the emergency department (ED), transferred care to the ED staff, including the amiodarone infusion simultaneously finishing during turnover.
The resident in charge of the patient said the patient was conscious alert and oriented; however, he was under the influence. His heart rate was 124 bpm after a 2nd dose of 150mg Amiodarone over 15 minutes. He had admitted to using drugs, and said: “he was a shaman, and that money was all that mattered in life.” The patient was discharged in the morning from the ED, having suffered no ill effects from his defibrillations. He admitted to illicit drug use.
Summarizing, this is a cautionary tale of the dangers of latching onto a diagnosis, i.e., a cardiac tachydysrhythmia as the cause rather than a symptom of a patient’s condition. The patient was in his mid-30s. Had a full history been able to be completed, it would have been readily apparent the patient was suffering from stimulant abuse. The best treatment the patient received was Versed. If I reran this call, I would consider the overall picture. How can the patient be altered from his heart rate if the blood pressure is okay? ETCO2 could have been applied to measure the level of perfusion with the lungs, and thus cardiac output. The stroke volume may be significantly reduced. While the patient may be altered and not responding, his collapse was witnessed by the callers, meaning this was a new onset state. The repeated inappropriate defibrillation did not assist the patient. Although it is interesting to note the amount of energy the patient was able to withstand without going into ventricular fibrillation. Is it possible the stimulant taken by the patient had a protective effect? Including increasing its automaticity and excitability. The amiodarone, with its impact on a variety of ion channels, would reduce the heart rate regardless as proven by the initial dose by EMS and the subsequent treatments in the ED.
Case reviews are presented in this post because there is something that can be learned from them. The recommendations made are for this particular patient condition and are submitted for learning purposes only and should not be considered a standard of care. You should always review and follow approved patient care protocols and practice good clinical decision making.